Many people who suffer from incontinence or specifically urinary incontinence (Latin: Incontinentia urinae) are ashamed of their illness. But in Germany about 6 to 8 million people are affected, women more often than men. Incontinence is characterized by various symptoms and can also be the result of a wide variety of diseases.
What is incontinence (urinary incontinence)?
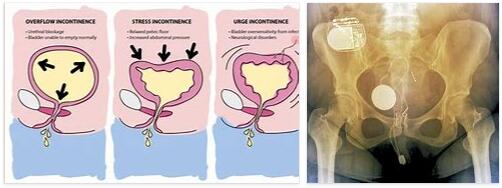
Schematic representation of the anatomy and structure of the urinary bladder.
According to abbreviationfinder, incontinence can take many forms. Common to all are problems with holding and self-determined delivery of urine. With increasing age, the probability of severe forms of incontinence increases.
In the case of urge incontinence, the patient suddenly feels the need to empty his bladder. In the case of stress incontinence, stress (coughing, sneezing, etc.) triggers an involuntary loss of urine.
In severe cases, simply standing up or even lying down can be a burden. Overflow incontinence is characterized by unintentional dribbling of urine. Reflex incontinence can result in the patient leaking urine without realizing it.
Causes
Incontinence can have many causes depending on the type of incontinence . In the case of urge incontinence, the patient has increased bladder sensitivity. The urinary bladder (detrusor) is permanently contracted and the patient feels the urge to urinate without the bladder being full.
Stress incontinence can be caused, among other things, by a functional weakness in the urinary tract. But especially in women, incontinence can also be caused by a weak pelvic floor. This weakness often occurs as a result of a general sagging of the internal organs due to weak ligaments and muscles and can be the result of a sudden birth.
Unconscious incontinence is characterized by obstructed drainage. These can be caused by an enlarged prostate. However, incontinence can also be caused by neurological diseases, diabetes or other reasons.
Symptoms, Ailments & Signs
Urinary incontinence can have different symptoms depending on the type and cause. Stress incontinence can be recognized by the fact that the involuntary loss of urine occurs mainly during physical exertion. The loss of urine can vary in intensity and typically occurs without a previous urge to urinate.
Urge incontinence is characterized by an acute, excessively strong urge to urinate before the urine suddenly escapes. This type of incontinence can occur several times an hour, even before the bladder is full. Overflow incontinence is when small amounts of urine leak out. Patients usually feel dribbling and a permanent urge to urinate.
Reflex incontinence is associated with irregular emptying of the bladder. Patients can no longer determine whether the bladder is full and usually do not empty the bladder completely. With extraurethral incontinence, urine is constantly being lost. This can be accompanied by pain in the area of the ureter and bladder.
In small children, urinary incontinence becomes noticeable by the fact that it occurs at irregular intervals and subsides by the age of four. If the symptoms persist well beyond the age of four, there is another form of urinary incontinence that needs to be diagnosed and treated by a doctor.
course of the disease
In many cases, treatment of incontinence is not only important for the patient’s quality of life, but can also be medically indicated.
Particularly in the case of an overflow bladder, failure to treat the incontinence can even lead to urinary poisoning (uremia) in the most severe cases.
The urine remaining in the bladder builds up in the ureter and kidneys and causes an increasing loss of function of the kidneys (renal insufficiency). This can then lead to serious consequences of urinary poisoning.
But the treatment of incontinence is also important in other cases. Incontinence can also be a symptom of another more serious condition, such as prostate cancer or diabetes. These diseases, which are accompanied by incontinence, usually worsen without treatment and can be fatal.
Complications
Urinary incontinence can be treated or managed well today. However, it also tends to leave room for various complications. Skin irritation may occur if urine comes into frequent contact with the skin. If left untreated, ulcers and inflammation can develop, especially in elderly or bedridden people.
Incontinence also increases the risk of urinary tract infection. In addition, those affected often feel embarrassed by their inability to hold their urine. In some cases, those affected can no longer hold their bowel movements. But even urinary incontinence can be a reason for many to withdraw from other people. They fear that the consequences of incontinence will become a disruptive factor in social life.
Psychological problems can occur as a complication of incontinence caused by surgery at a young age. Depression or anxiety can be an additional burden for those affected. In addition, not everyone has the opportunity to provide themselves with the necessary incontinence pads and aids.
Surgery can help with stress incontinence after childbirth or a hysterectomy. However, such operations can also lead to complications. Therefore, an attempt is first made to counteract urinary incontinence with a conservative treatment approach with pelvic floor exercises. Depending on the surgical method, wound healing disorders can occur. Postoperative bleeding, urinary tract infections, nerve irritation and damage can occur as a result of the operation. Peritonitis is possible but less common.
When should you go to the doctor?
Many patients with urinary or fecal incontinence avoid going to the doctor out of shame or fear of possible tests. Nevertheless, those affected who can no longer hold their urine or stool should be examined and advised as soon as possible. This is also recommended if it is only a mild form of urinary incontinence. As a rule, incontinence can be treated well after medical advice. Which type of therapy is suitable for the person concerned can only be determined if the treating doctor can determine the exact form of the incontinence by means of examinations.
In some cases, the incontinence can worsen significantly if left untreated. It usually does not go away on its own. Sometimes incontinence can also be a symptom of serious medical conditions. For this reason, it is advisable to consult a doctor as soon as possible after the symptoms appear. The sooner those affected take such measures, the higher the chances of recovery. It is advisable to consult your family doctor first.
Treatment & Therapy
The treatment of incontinence must always focus on the causes. The patient should seek advice from a doctor. In the case of a pelvic floor weakness, the first goal is of course to strengthen the pelvic floor muscles. This can be strengthened through a variety of exercises.
Biofeedback support is sometimes necessary so that the patient learns to control the muscle movements. For this purpose, a probe is inserted that shows which muscle is being contracted at the moment. Occasionally, in the case of stress incontinence, estrogen treatment or, in severe cases, the formation of an artificial sphincter makes sense. In mild cases of urge incontinence, bladder teas, medicines made from herbal ingredients and heat treatment can have an effect.
You can also reduce incontinence with toilet training. For this purpose, the patient goes to the toilet at predetermined times and thus forestalls the urge. In more severe cases, advice can also be given on the administration of stronger medication against the incontinence.
In many cases, unconscious incontinence can be alleviated by herbal medicines made from pumpkin, nettle or saw palmetto. In severe cases, administration of an alpha-receptor blocker is also useful. This loosens the bladder seal and lowers the outflow resistance and can thus combat incontinence.
Outlook & Forecast
The prognosis of incontinence is linked to the age of the patient and the existing underlying disease. Depending on the disorder present, spontaneous healing or chronic development of the disease can occur.
In children, incontinence occurs during nighttime sleep as part of the natural growth and development process. Control of the sphincter must first be trained sufficiently before it can function properly. It is a temporary phenomenon with sporadic occurrence, which usually occurs by the age of six. During this time there may be phases when you are free of symptoms. Then a spontaneous end to the wetting is to be expected.
In older people, the muscles naturally weaken. Incontinence occurs, which in most cases remains until the end of life. There is no prospect of recovery in these patients.
If the incontinence is triggered by paralysis or a viral disease, the prognosis of the causative disease must be taken into account. This is decisive for the further course and the prospect of alleviation or healing of the symptoms. If existing germs can be found and treated with medication, recovery occurs within a few days or weeks. If the muscles are paralyzed, it is often no longer possible to be free of symptoms.
Prevention
Strengthening the pelvic floor muscles is an effective way of preventing incontinence, especially for women. Many adult education centers and sports clubs offer special exercises.
But a healthy lifestyle also significantly reduces the risk of incontinence. In general, to prevent incontinence, one should pay attention to a healthy diet, not smoke and fight any existing obesity.
Aftercare
Patients need extensive support with incontinence care in their everyday life. Continuous monitoring and advice from a specialist and trained medical staff in the field of stoma care and therapy is important here. In order not to always be afraid of an indisposition in everyday life, it is necessary and recommended for patients to use suitable pads, pads or diapers.
The templates are characterized by their size and absorbency and are therefore also differentiated for day and night use. With the appropriate expert advice, the patient will find the right incontinence material for himself, so that he can get through the day and night with as few restrictions as possible. However, it is necessary to change the patient’s incontinence material in good time in order to avoid unpleasant odors or anything visible.
With individually adapted incontinence care, participation in social life is almost unrestricted. In addition, measures and therapies should take effect that can improve continence in the long term. This includes strengthening the muscles through targeted pelvic floor training. However, patients need patience, initiative and perseverance for this. An improvement may only appear after weeks or months, since the muscles first have to strengthen and develop.
You can do that yourself
Targeted gymnastic exercises strengthen the pelvic floor muscles and can significantly reduce the involuntary loss of urine in mild forms of incontinence. However, they must be carried out consistently and continuously in order to achieve a long-lasting effect. Reducing obesity and eating a high-fiber diet also has a positive effect on the pelvic floor muscles.
In many cases, bladder training is helpful, in which the bladder is emptied regularly at certain times before a strong urge to urinate sets in. Nocturnal urine leakage can often be avoided by planning one or two visits to the toilet. Drinking less in the case of urinary incontinence is usually counterproductive: due to the reduced amount of urine, the urinary tract is no longer flushed out sufficiently, bacteria can multiply and cause urinary tract infections. These in turn cause a constant urge to urinate, which in turn is accompanied by uncontrolled urination.
In order not to slip into social isolation, those affected should continue their everyday life as normally as possible despite the urinary incontinence and also not forgo their usual leisure activities: Discreet but very absorbent pads provide security at work and during sports, with special incontinence swimwear are also Swimming pool visits easily possible. Anyone who suffers severely from incontinence should not be afraid to seek talks with a psychologist, psychotherapist or in a self-help group.