A disc degeneration or disc wear is characterized by wear of discs. A main therapeutic focus is on combating symptoms that occur.
What is intervertebral disc degeneration?
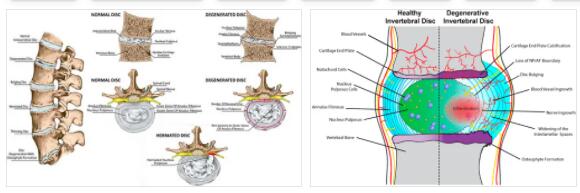
Disc degeneration is wear and tear on the intervertebral discs (the cartilage intervertebral discs in the spine).
In the course of intervertebral disc degeneration abbreviated as IDD by AbbreviationFinder, the intervertebral discs become thinner and more cracked, so that they are less able to buffer the vertebral bodies against each other. This places increased stress on the vertebral bodies. In most cases, the intervertebral discs in the lumbar and / or cervical spine are affected by disc degeneration.
Typical complaints that are often associated with intervertebral disc degeneration are local back pain, which can be exacerbated by muscle tension. The risk of suffering a herniated disc (parts of a disc protrude between the vertebrae) also increases with disc degeneration.
Causes
Not only various pathological processes can lead to intervertebral disc degeneration – with increasing age, the intervertebral discs increasingly lose the ability to absorb water, so that the cartilage tissue becomes less elastic.
Due to the increasing porosity of the intervertebral discs, cracks also frequently occur in the intervertebral disc; disc degeneration sets in. Age-related degeneration of the intervertebral discs can also be favored by factors such as a lack of physical exercise and long-term heavy pressure loads on the spine. Such an increase in pressure is caused in the lumbar spine area, for example, by heavy carrying or by lifting with the trunk bent forward.
The diseases and injuries that can cause or promote disc degeneration include, for example, fractures (ruptures) of the vertebral bodies. Deformities of the spine, such as those present in the context of scoliosis (curvature of the spine), also promote degeneration of the intervertebral discs.
Symptoms, ailments & signs
Disc degeneration manifests itself through various symptoms and complaints, which depend on the extent and location of the wear and tear. An acute protrusion of the intervertebral disc manifests itself as local back pain that sometimes extends to the abdomen or sternum. A herniated disc causes dysfunction of the bladder and rectum as a result of compression.
It can also cause pain, which increases when you cough, sneeze or strain. In most cases, there is also a protective posture of the relevant spinal column section, which can be expressed, for example, by a stooped posture or a hollow back. In the case of chronic disc degeneration, the vertebral joints are heavily stressed, which can lead to local pain symptoms.
The pain is usually accompanied by psychological and psychosomatic complaints. Many sufferers suffer from mood swings, depressive moods and a general malaise. The limitations in mobility can cause further discomfort. This can lead to further wear and tear on the surrounding joints.
Also circulatory disorders, sensory disturbances and paralysis can not be excluded. Furthermore, muscle tension and hardening can occur. If the intervertebral disc degeneration is based on an acute injury such as a rupture, further symptoms and complaints may arise in some cases.
Diagnosis & course
In order to diagnose disc degeneration, a treating specialist (e.g. an orthopedic surgeon) usually asks for facts such as the type and approximate start of the symptoms. After a physical examination, possible diagnostic methods to be used are, for example, X-rays or MRI (magnetic resonance tomography).
While the X-ray method is well suited for diagnosing intervertebral disc degeneration, in order to show the bony structure of the vertebral bodies, magnetic resonance imaging is suitable, among other things, for showing nervous structures that run in the vertebral canal and that can be affected by intervertebral disc degeneration. A degeneration of the intervertebral disc can typically be recognized on the basis of x-rays, for example by a reduction in the affected intervertebral spaces.
The course of intervertebral disc degeneration varies from person to person and depends, among other things, on factors such as the corresponding causes and measures taken against the degenerative symptoms. As a rule, intervertebral disc degeneration is insidious and often does not immediately lead to symptoms. When the first symptoms appear varies from person to person.
Complications
In the case of intervertebral disc degeneration, there is qualitative wear and tear on the intervertebral disc tissue. Important fluid, which the fine supporting cartilage tissue needs, can no longer be stored. The vertebral bodies become more porous and lose their buffer function. The symptom can appear in the lumbar as well as the cervical spine.
A distinction is made between age-related or accident-related degeneration due to vertebral fractures, constitutional curvature of the spine and athletes and people with one-sided occupational stress. Disc degeneration can cause various life-impairing complications.
This includes extensive pain states that show themselves in everyday executions such as stooping, sneezing, coughing, pressing or in a state of rest. If left untreated, the symptom can become chronic in the form of a bulging disc. The space between the vertebrae shrinks and there is a threat of prolapse with loss of vegetative functions in the lower or upper body area.
Diagnostic imaging procedures help with the medical examination to determine to what extent the damage to the intervertebral discs and the nervous structures has progressed. Then the cause is treated. However, damage to the cartilage tissue that has already occurred cannot be regenerated. The medical measures serve to alleviate pain with physiotherapeutic strengthening of the muscle tissue supporting the spine.
Surgical measures only take place when important body functions are acutely blocked. The stiffening or intervertebral disc prosthesis can reduce pain, but as a consequence of complications, further disc degeneration can develop near the operated site as the patient ages.
When should you go to the doctor?
If your back pain or muscle tension increases, you should always consult a doctor. Anyone who has ever suffered a herniated disc or the like should speak directly to the responsible specialist.
If the pain increases rapidly and is associated with acute symptoms such as lumbago, it is advisable to go to the nearest hospital. The same applies if the symptoms mentioned occur increasingly during everyday processes such as bending over, sneezing or coughing. If the pain leads to misalignment, a doctor must be consulted.
The doctor can clarify unequivocally whether it is a question of intervertebral disc degeneration and then refer the person concerned to an appropriate specialist. Depending on the diagnosis this makes, further examinations must then be carried out. In the case of intervertebral disc degeneration, further examinations and surgical treatment should be carried out promptly. Otherwise, chronic pain, misalignments and other sequelae can occur, which can be a lifelong burden for those affected.
Treatment & Therapy
If intervertebral disc degeneration was caused or promoted by existing diseases / injuries to the spine, an important therapeutic goal is usually treatment of the cause. With a correspondingly consistent treatment of the cause, the favored intervertebral disc degeneration can often also be positively influenced.
Since damage to the cartilage tissue that has occurred in the context of intervertebral disc degeneration cannot be reversed, symptomatic treatment (such as relieving pain) plays an important role. Corresponding pain can be counteracted by individually tailored physiotherapeutic (physiotherapy) measures.
Avoiding heavy carrying and possibly reducing excess weight can also help relieve pain. In the case of severe pain in the context of intervertebral disc degeneration, pain-relieving medication can also be used after consulting the attending physician.
Surgical measures can be useful, for example, if the back pain caused is chronic; if they have lasted for at least a few months without subsiding in the meantime. Depending on the patient, surgical treatment of a generation of intervertebral discs offers the possibility of a disc prosthesis or so-called spondylodesis (stiffening) – in this case the affected vertebral segment is stiffened in order to achieve freedom from pain.
Outlook & forecast
Disc degeneration usually has an unfavorable prognosis. Nevertheless, the severity of the disease is individual and can lead to very minor restrictions in everyday life in some patients.
The course of the disease is gradually increasing. The wear and tear is fundamentally part of a natural process over the life span. The symptoms are, however, dependent on the physical strain, the genetic requirements and the lifestyle of the patient.
With good conditions, a healthy lifestyle and the observance of various medical tips, the progress of the disease can be delayed for a long time. Targeted training and exercises help to put the right load on the body and to coordinate movements optimally. The signs of wear and tear are often hardly noticed by these patients or can be compensated for by a correct and healthy posture.
In people with a high dead weight and a professional or sporting activity that leads to a heavy load on the skeleton, the symptoms often increase rapidly. You need a restructuring of your everyday life and are asked to relieve your body as much as possible immediately.
Surgical intervention can significantly alleviate the complaint. However, a natural possibility of movement or a familiar load limit is not achieved. Nevertheless, the quality of life and general well-being increase significantly with treatment of the intervertebral disc.
Prevention
Age-related disc degeneration can only be prevented to a limited extent. However, the degeneration process can be slowed down by measures such as physical exercise, little pressure on the spine and avoiding / combating obesity. Early treatment of diseases / injuries that can lead to intervertebral disc degeneration can often counteract such degenerative processes.
Aftercare
Disc degeneration can be treated conservatively and surgically. Both treatment options require good aftercare in order to optimize regeneration and ensure the success of the therapy. Once an operation has been carried out, follow-up care begins with wound care and mobilization, which, in collaboration with doctors and specialists such as physiotherapists, also requires active cooperation on the part of the patient.
Initially, the patient is only allowed to lift certain weights, which must be strictly adhered to in order not to overload the affected region of the spine. Getting out of bed in a back-friendly manner is also very important and must be built into everyday life. The back school shows patients exactly what back-friendly behavior looks like in everyday life.
Correct lifting and carrying is also discussed, as is sleep, which requires a back-friendly mattress. Therefore, back training is a very important factor in aftercare, regardless of the previous form of treatment. Muscular imbalance and obesity are often factors in the development of intervertebral disc degeneration. Conversely, this means that aftercare also means balancing out muscular imbalances and reducing weight.
Muscles that are weakened need to be strengthened. This often affects the abdominal muscles and upper back. Muscles that are shortened, on the other hand, have to be stretched. Weight reduction can be achieved particularly well through endurance sports. Back-friendly variants such as walking or backstroke swimming are recommended here. Rehabilitation sport shows the patient which sport can be used specifically.
You can do that yourself
In everyday life, the degeneration of the intervertebral discs is often a hindrance with the usual movement sequences. Even if people experience pain, they should take a pain reliever and stay active. Only in very acute phases is it advisable to rest for a short time in order to prevent possible inflammatory processes or further nerve irritation.
The activity should primarily consist of endurance sports that strengthen the back muscles. Swimming is particularly suitable, as it optimally trains the back, pain in the water is alleviated and those affected sometimes find the cooling by the water to be pleasant and relieving. In addition, the body weight then does not rest on the intervertebral discs. Sports in which the entire pressure is cushioned via the intervertebral discs and the spine are less recommended. This is especially the case when jogging. Cycling is better then.
Wearing support belts should only be used for a very short time. The muscles are quickly weakened by wearing, as is the case with rest when pain interferes with movement. Those affected can also make use of the medical offers. These consist in particular of physiotherapy and functional training.
In individual cases, of course, the cause of the intervertebral disc degeneration must always be included and the help optimally tailored to the individual patient.