The parietal foramen is an opening on the upper edge of the so-called parietal bone on the skull. The parietal emissary vein, which connects to the superior sagittal sinus, and a secondary branch of the occipital artery pass through it. The presence and size of such foramina differs from person to person. While in some people there is no parietal foramen at all, a congenital foramen parietal permagnum disease leads to an abnormal enlargement of the same.
What is Parietal Permagnum Foramen?
According to TOPBBACOLLEGES.COM, a parietal permagnum foramen is a rare, congenital cranial bone defect based on a gene mutation. This is usually located on both sides of the parietal bone about one centimeter lateral to the sagittal suture and above the lambdoid suture.
The main apparent feature is a considerable enlargement of normal parietal foramina, which physiologically occurs in around 65 percent of the population. A foramen parietale permagnum can have a size between at least five millimeters up to several centimeters. The prevalence is around 1: 15,000 to 1: 25,000.
Causes
The dysplasia of the skull bone is genetic in this case and can be traced back to certain gene mutations. The basic defect of the local ossification disorder is still unknown. However, it is known that inheritance is autosomal dominant.
Foramina parietalia permagna can be classified into different groups depending on which mutation is underlying which gene in each case. If there is a mutation in the MSX2 gene at gene location 5q35.2, this foramen belongs to group 1. If, on the other hand, there is a mutation in the ALX4 gene at 11p11.2 5q35.2, this oversized foramen is assigned to class 2.
There is also a third group in which, however, no specific mutation has yet been found in a particular gene locus. A parietal permagnum foramen per se has basically no disease value to speak of. However, it is often associated with a more complex syndrome, such as Saethre-Chotzen syndrome, also known as acrocephalosyndactyly type 3] (ACPS 3).
Symptoms, ailments & signs
A foramen parietale permagnum is characterized by an oval or rounded opening in the parietal bones about five centimeters in size in adulthood, which can be present either on one or both sides and is closed by membranes. A mongoloid lid axis position is very common. Occasionally headaches and / or absenteeism occur, but these are very unspecific symptoms.
The large foramina are often associated with a cleft lip and palate. Scalp abnormalities or local alopecia can also occur. Studies have shown that in a clan with three consecutive affected generations, a parietal permagnum foramen occurs in combination with ptosis, i.e. the partial or complete drooping of an eyelid.
In addition, other skull bones may also be involved, for example a cranium bifidum. The most common complications include severe headaches, in particular, which can affect the quality of life. Taken alone, however, foramina parietalia permagna have essentially no clinical significance.
This only happens when they are accompanied by syndromes. Possible syndromes include FG syndrome, Potocki-Shaffer syndrome, Ritscher-Schinzel syndrome, multiple cartilaginous exostoses, and Toriello syndrome.
Diagnosis
Thanks to today’s modern examination methods, FPPs can be diagnosed very early in the unborn child during gestation. Sometimes, however, these are also incidental findings in adulthood. During a clinical examination, the openings are often palpable as a flattened region or as an enlarged posterior fontanel.
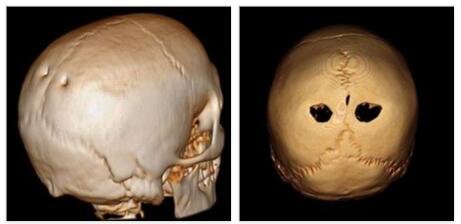
The openings are clearly visible in an anterior-posterior x-ray. However, it is often more difficult to identify a permagnum parietal foramen on a lateral radiographic image. A CT imaging, 3D reconstruction can delimit the osseous defect very accurate and a magnetic resonance imaging (MRI) can make any intracranial changes visible.
If the FPP is accompanied by anomalies in the vessels, vascular imaging is also helpful. A prenatal diagnosis during pregnancy is recommended for families with a known genetic defect that can be associated with foramina permagna.
This prenatal diagnosis is carried out between the 18th and 20th week of pregnancy and includes neurosonography as part of further ultrasound diagnosis, as well as molecular genetic diagnosis for the genes MSX2 and ALX4. The course of the disease is usually aymptomatic and benign, but spontaneous closure is extremely unlikely.
Complications
In most cases, there are no specific symptoms or complaints due to the Foramen Parietale Permagnum. For this reason, the diagnosis of the parietal permagnum foramen is made relatively late, which means that early treatment is not possible. Those affected suffer from headaches, which occur only sporadically and are not permanent. Confusion can also arise, although this is also not permanent.
It is not uncommon for patients to suffer from a cleft palate, which significantly reduces their quality of life. One of the two eyelids hangs down. The headache often leads to depression or other psychological upsets. It is not uncommon for those affected to suffer from exhaustion or irritability and no longer actively participate in life.
As a rule, the affected person is also restricted in his everyday life by the foramen parietale permagnum, so that certain dangerous sports should not be carried out. The disease can also be treated with surgery. There are no complications and there is no reduction in life expectancy.
When should you go to the doctor?
A doctor should be consulted in the case of the parietal permagnum foramen. This complaint can lead to significant restrictions in everyday life. Early treatment is necessary, especially in children, so that developmental disorders do not occur.
The doctor should be seen if there is an opening in the parietal bone. Severe headaches or a misalignment of the head can also indicate the Foramen Parietale Permagnum and should be examined. In some cases, those affected also suffer from a cleft palate, although this is recognized and treated at birth.
In most cases, the Permagnum Parietal Foramen only causes pain in the head or neck. If this pain significantly restricts everyday life and reduces the quality of life of the person affected, a visit to the doctor is recommended. The disease is treated by a general practitioner or an orthopedic surgeon.
Most of the time, this can alleviate the symptoms. With the Foramen Parietale Permagnum, however, the person affected should refrain from dangerous sports or activities that have an increased risk of accidents. In most cases, the disease progresses positively with this disease.
Treatment & Therapy
Treatment for an enlarged parietal foramen is mostly conservative. A persistent cranium bifidum, however, justifies an operative intervention for the closure. Possible associated headaches and seizures can be treated with medication.
The risk of penetrating brain injury is small, but it can cause anxiety in patients and loved ones, so good education about the abnormality of the skull is very important. Parents, affected children and teachers should be well informed about the clinical picture.
This enables them to avoid risky behaviors that could lead to such an injury, such as contact sports, if possible. Cranioplasty is only considered for groups at risk for skull injuries, such as active children, but the use of such an operation is still controversial.
Outlook & forecast
The disease is based on a genetic defect. Due to legal requirements, human genetics must not be changed. For this reason, symptomatic treatment takes place. The prognosis of the Foramen Parietale Permagnum depends on the extent of the existing complaints. Complete freedom from symptoms is not to be expected.
If the irregularities such as headaches or cramps occur sporadically and not very strongly in the patient, drug therapy is used. As soon as the impairments show up in the course of life, the active ingredients in the medicines alleviate the existing symptoms until recovery occurs after a while.
These patients report periods of complete recovery and periods in which an increase in symptoms can be observed. Often the developments are dependent on the lifestyle and the developments in the immediate environment of the person concerned.
In severe cases, surgery is performed. The skullcap is closed in this. Operations are always associated with various risks and side effects. If complications arise, the prognosis for the patient worsens. If the procedure is successful, there will be rapid improvement in general health. Headache or seizure disorders subside. However, some limitations are necessary in the course of life. Since the risk of injury is increased, the skullcap must be protected from outside influences.
Prevention
The most important measure to prevent complications is adequate education of those affected and those around them. Risky physical activity or other dangerous behavior should be avoided as much as possible.
If the skull bone defect is diagnosed prenatally, the next steps must be planned and discussed with the pregnant woman. An elective caesarean section, for example, reduces the risk of traumatic injury to the brain during the birth process.
Aftercare
In the case of the Foramen Parietale Permagnum, in most cases there are no options for follow-up care. However, these are not really necessary, as the disease can be treated completely and without complications through a surgical procedure. After the treatment, the symptoms disappear completely.
The earlier the Foramen Parietale Permagnum is detected, the more successful is the further course of this disease in most cases. Therefore, a doctor should be consulted with the first symptoms that indicate the disease. In most cases, foramen parietale permagnum, surgery is performed on the skull to completely alleviate the symptoms.
Since this is a relatively serious and complicated procedure, the patient should definitely rest afterwards and not strain his body unnecessarily. Bed rest should be observed, and stressful activities should also be avoided. Children should be informed by their parents before the procedure so that they do not lead to unnecessary feelings of fear or other psychological upsets.
The care and support in everyday life from your own family or friends is always helpful and usually accelerates healing. Successful treatment of the Parietale Permagnum Foramen does not reduce the patient’s life expectancy either.
You can do that yourself
To improve the quality of life, the patient should avoid anything that could cause headaches or discomfort of the skull. Stress should be reduced and physical overexertion should also be avoided. Hustle and bustle and haste often lead to internal tension, which has a negative impact on the organism. Brooding and disputes should be avoided so that there is no internal pressure build-up. As soon as the first headaches appear, rest and protection are important.
Getting enough sleep, drinking enough fluids and avoiding loud ambient noises help to alleviate the symptoms. When dealing with the visual anomalies of the disease, it is important to be very self-confident. The use of cover accessories or cosmetic tricks may find application. In most cases, an open approach to the disease results in acceptance by people from the closer social environment, so that the use of accessories can increasingly be dispensed with.
In addition, discussions with therapists, relatives or other sick people help to gain awareness of the environment. This often leads to cognitive changes and changes in one’s own attitude, as many worries turn out to be unnecessary. The exchange with other people also helps to reduce fears.